Tuberculosis Outbreak In Kansas City
As of January 31, 2025, Kansas city in USA is experiencing a significant tuberculosis (TB) outbreak, primarily affecting the Kansas City metropolitan area. According to KDHE -The Kansas Department of Health and Environment ‘outbreak is larger than normal for Kansas, the risk remains low for the general’. KDHE public reports 67 confirmed active TB cases—60 in Wyandotte County and 7 in Johnson County. Additionally, there are 79 confirmed latent TB infections in the region.
This outbreak, which began in early 2024, has resulted in two fatalities. Health officials emphasize that the risk to the public remains low, as TB typically requires prolonged close contact for transmission. The KDHE, in collaboration with local health departments and CDC is actively conducting case investigations, contact tracing, and public health education to manage and contain the outbreak.
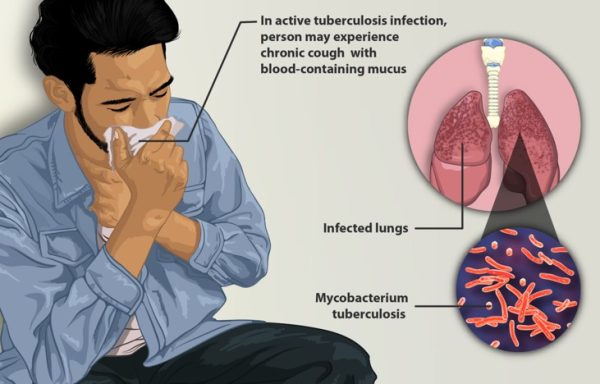
TB is an airborne bacterial infection that primarily affects the lungs. Symptoms of active TB include a persistent cough, chest pain, and fatigue. While TB is treatable with antibiotics, the treatment regimen is lengthy, often requiring several months of medication adherence. Individuals diagnosed with active TB are undergoing treatment, and many have completed their therapy successfully.
The KDHE continues to monitor the situation closely and advises residents to remain informed through official public health channels. Healthcare providers are reminded to report suspected TB cases promptly to facilitate timely public health interventions.
Do you know? Tuberculosis (TB) has been present in humans for thousands of years, but it was discovered as a bacterial disease in 1882 by Dr. Robert Koch, a German physician and microbiologist. He identified the bacterium responsible for TB, Mycobacterium tuberculosis, and presented his findings on March 24, 1882. This discovery was groundbreaking because it provided scientific proof that TB was caused by a specific microorganism, paving the way for further research, diagnosis, and treatment.Before Koch’s discovery, TB was known by various names, such as “consumption” or “phthisis,” and had been documented in ancient Egyptian mummies, indicating its presence for at least 4,000 years.
Tuberculosis (TB) symptoms and treatment :
Symptoms of TB :TB is a bacterial infection caused by Mycobacterium tuberculosis, primarily affecting the lungs but sometimes spreading to other organs. It can be active (symptomatic and contagious) or latent (dormant and non-contagious).
Symptoms of Active TB:
- Persistent cough (lasting more than three weeks)
- Coughing up blood or mucus
- Chest pain or pain when breathing and coughing.
- Fever and night sweats
- Unexplained weight loss
- Loss of appetite
- Fatigue and weakness
Symptoms of Latent TB:
- No symptoms (the bacteria are present but inactive)
- Not contagious, but it can become active later.
Prevention and public health measures:
- BCG vaccine (given in some countries, but not widely used in the U.S.)
- Early detection and treatment of infected individuals
- Wearing masks and good ventilation in high-risk areas
- Regular screening for healthcare workers and those in close contact with TB patients
What is the treatment for TB? Is it curable?
TB is treatable and curable with antibiotics, but treatment must be followed strictly to prevent resistance.
Standard treatment for Active TB: A 6-month regimen of antibiotics, typically:
- First 2 months (Intensive Phase): Rifampin (RIF), Isoniazid (INH), Pyrazinamide (PZA) Ethambutol (EMB)
- Next 4 months (Continuation Phase): Rifampin (RIF) Isoniazid (INH)
Treatment for Latent TB: Isoniazid (INH) for 6-9 months, Rifampin (RIF) for 4 months and Combination therapy (INH + Rifapentine) for 3 months
Who is at high risk for TB? Certain groups of people should be especially careful about tuberculosis (TB) because they are at higher risk of infection or developing active TB disease. These include:
1. People with weakened immune systems:
- HIV/AIDS patients – TB is a leading cause of death among people with HIV.
- Cancer patients – Those undergoing chemotherapy or radiation therapy.
- Organ transplant recipients – Taking immunosuppressive drugs increases susceptibility.
- People with autoimmune diseases – Those on biologic drugs for conditions like rheumatoid arthritis or lupus.
- Diabetics – Poorly controlled diabetes increases TB risk.
- Malnourished individuals – A weakened immune system makes it harder to fight off TB.
2. Close contacts of TB patients: Family members, roommates, or healthcare workers exposed to TB patients. And People living in overcrowded places like prisons, homeless shelters, or refugee camps.
3. Elderly individuals: Weakened immune function with age makes TB more dangerous.
4. Smokers and heavy alcohol/drug users: Smoking damages the lungs, making them more vulnerable. Excessive alcohol and drug use weaken the immune system.
5. Healthcare workers: High exposure risk due to contact with infected patients.
6. Travelers to high-TB regions: Countries with high TB rates include India, China, South Africa, Indonesia, and parts of Eastern Europe.
Since TB treatment requires months of strict adherence, directly observed therapy (DOT) is often recommended, where healthcare providers monitor patients taking their medications to ensure successful treatment.
References:
- kdhe.ks.gov
- https://www.who.int/news-room/fact-sheets/detail/tuberculosis
- https://www.cdc.gov/tb/about/index.html
- https://www.lung.org/lung-health-diseases/lung-disease-lookup/tuberculosis/learn-about-tuberculosis
Image credit: https://www.myupchar.com/, CC BY-SA 4.0 <https://creativecommons.org/licenses/by-sa/4.0>, via Wikimedia Commons
Author: Sumana Rao | Posted on: February 7, 2025
« Guillain Barre Syndrome Measles Outbreak Continues In Rural West Texas »




















Write a comment