Malnutrition
- Definition
- Symptoms of malnutrition
- Children
- What causes malnutrition?
- Management (in India)
- Diagnosis
- MUST (Malnutrition Universal Screening Tool)
- Preventing malnutrition
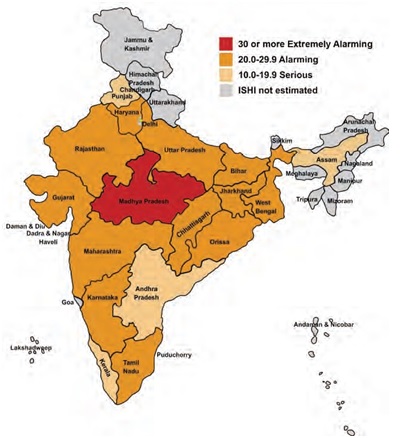
Image Courtesy: http://www.motherchildnutrition.org/india/index.html
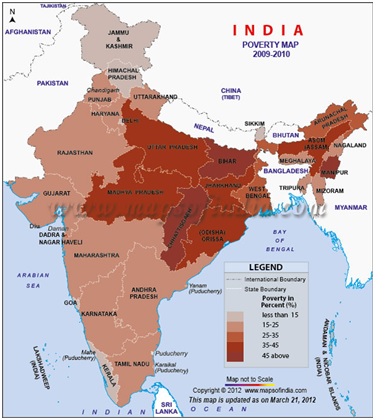
Image courtesy: http://blog.mapsofindia.com/india/eradication-of-poverty-in-india-is-it-a-distant-dream-for-us/
Definition:
Malnutrition is a broad term which refers to both under nutrition and over nutrition.
Under nutrition occurs when an individual does not consume enough food. It may exist if the person has a poor diet that gives them the wrong balance of basic food groups.
Obese people, who consume more calories than they need, may suffer from the sub nutrition aspect of malnutrition if their diet lacks the nutrients their body needs for good health.
The World Health Organization (WHO) says that malnutrition is by far the largest contributor to child mortality globally, currently present in 45 percent of all cases.4
Underweight births and inter-uterine growth restrictions are responsible for about 2.2 million child deaths annually in the world. Deficiencies in vitamin A or zinc cause 1 million deaths each year.
WHO adds that malnutrition during childhood usually results in worse health and lower educational achievements during adulthood. Malnourished children tend to become adults who have smaller babies.
While malnutrition used to be seen as something which complicated such diseases as measles, pneumonia and diarrhea, it often works the other way round – malnutrition can cause diseases to occur.
Globally, as well as in developed, industrialized countries, the following groups of people are at highest risk of malnutrition (subnutrition):
- Elderly people, especially those who are hospitalized or in long-term institutional care
- Individuals who are socially isolated
- People on low incomes (poor people)
- People with chronic eating disorders, such as bulimia or anorexia nervosa
- People convalescing after a serious illness or condition
Deficiencies in nutrition inflict long-term damage to both individuals and society. Compared with their better-fed peers, nutrition-deficient individuals are more likely to have infectious diseases such as pneumonia and tuberculosis, which lead to a higher mortality rate. In addition, nutrition-deficient individuals are less productive at work. Low productivity not only gives them low pay that traps them in a vicious circle of under-nutrition, but also brings inefficiency to the society, especially in India where labour is a major input factor for economic production. On the other hand, over-nutrition also has severe consequences. In India national obesity rates in 2010 were 14% for women and 18% for men with some urban areas having rates as high as 40%.Obesity causes several non-communicable diseases such as cardiovascular diseases, diabetes, cancers and chronic respiratory diseases.
Symptoms of malnutrition:
Symptoms of malnutrition include:
- Loss of fat (adipose tissue)
- Breathing difficulties, a higher risk of respiratory failure
- Depression
- Higher risk of complications after surgery
- Higher risk of hypothermia – abnormally low body temperature
- The total number of some types of white blood cells falls; consequently, the immune system is weakened, increasing the risk of infections.
- Higher susceptibility to feeling cold
- Longer healing times for wounds
- Longer recover times from infections
- Longer recovery from illnesses
- Lower sex drive
- Problems with fertility
- Reduced muscle mass
- Reduced tissue mass
- Tiredness, fatigue, or apathy
- Irritability.
In more severe cases:
- Skin may become thin, dry, inelastic, pale, and cold
- Eventually, as fat in the face is lost, the cheeks look hollow and the eyes sunken
- Hair becomes dry and sparse, falling out easily
- Sometimes, severe malnutrition may lead to unresponsiveness (stupor)
- If calorie deficiency continues for long enough, there may be heart, liver and respiratory failure
- Total starvation is said to be fatal within 8 to 12 weeks (no calorie consumption at all).
Children
Children who are severely malnourished typically experience slow behavioral development, even mental retardation may occur. Even when treated, undernutrition may have long-term effects in children, with impairments in mental function and digestive problems persisting – in some cases for the rest of their lives. Adults whose severe undernourishment started during adulthood usually make a full recovery when treated.
In India malnutrition in children commonly happens because of
- cause lack of appetite
- disrupt the normal process of digestion
- cause the body to have an increased demand for energy
- Childhood diseases : diarrhea, vomiting, allergy, inadequate food intake
- poverty
- Far away education institutes
- Lack of physical activity
- Stress and avoiding eating due to issues with their body image.
What causes malnutrition?
Malnutrition, the result of a lack of essential nutrients, resulting in poorer health, may be caused by a number of conditions or circumstances. In many developing countries long-term (chronic) malnutrition is widespread – simply because people do not have enough food to eat. In more wealthy industrialized nations malnutrition is usually caused by:
- Poverty: Regardless of all the reasons contributing to poverty in India, India is at present adding population of 40 million people to the middle class annually.
According to the 2011 Global Hunger Index (GHI) Report, India ranks as one of the three nations where the Global Hunger Index from 1996 to 2011 rose to 23.7 from 22.9. At the same time, a survey was conducted taking into consideration 78 out of the 81 developing nations across the world such as Nepal, Pakistan, Vietnam, Bangladesh, Nigeria, Kenya, Uganda, Myanmar, Malawi, and Zimbabwe that have been successful in bettering the hunger situation. The most recent information provided by UNICEF demonstrates that one out of three kids who are suffering from malnutrition all over the world will be found In India. At the same time, around 42% of the kids of the country below the age of five years are underfed. The report also comes up with the fact that around 58% of the kids below the age of five years were underdeveloped. According to Rohini Mukherjee, one of the officials of the Naandi Foundation, the performance of India in hunger management is even poorer than the nations that form sub-Saharan Africa. The Naandi Foundation is one of the charitable non-governmental organizations that are working to eradicate poverty in India.
What are the causes of Poverty in India? The causes behind poverty in India are manifold. Some of the major causes include license raj, absence of market economy, red tapism, the negative outcomes of liberalization policies, and centralization of industries.
Given below are the different problems and issues that give rise to poverty among most of the people of the country:
- It is oftentimes difficult for the citizens of India or nearly impossible to get accessibility to essential amenities such as electricity, drinking water, healthcare and public transport.
- One of the most significant concerns for a big nation like India is the trouble to access the basic services.
- Approximately half of the manpower of the country relies on agricultural and cultivation activities.
- The middle class is mostly affected by the food inflation, and echoes of dissatisfaction are rising among them.
( See more at: http://blog.mapsofindia.com/india/eradication-of-poverty-in-india-is-it-a-distant-dream-for-us/#sthash.FHjMaFxN.dpuf)
- Poor diet – if a person does not eat enough food, or if what they eat does not provide them with the nutrients they require for good health, they suffer from malnutrition. Poor diet may be caused by one of several different factors. If the patient develops dysphagia (swallowing difficulties) because of an illness, or when recovering from an illness, they may not be able to consume enough of the right nutrients.
- Mental health problems – some patients with mental health conditions, such as depression, may develop eating habits which lead to malnutrition. Patients with anorexia nervosa or bulimia may develop malnutrition because they are ingesting too little food.
- Mobility problems – people with mobility problems may suffer from malnutrition simply because they either cannot get out enough to buy foods, or find preparing them too arduous.
- Digestive disorders and stomach conditions – some people may eat properly, but their bodies cannot absorb the nutrients they need for good health. Examples include patients with Crohn’s disease or ulcerative colitis. Such patients may need to have part of the small intestine removed (ileostomy). Individuals who suffer from Celiac disease have a genetic disorder that makes them intolerant to gluten. Patients with Celiac disease have a higher risk of damage to the lining of their intestines, resulting in poorer food absorption. Patients who experience serious bouts of diarrhea and/or vomiting may lose vital nutrients and are at higher risk of suffering from malnutrition.
- Alcoholism – this is a chronic (long-term) disease. Individuals who suffer from alcoholism can develop gastritis, or pancreas damage. These problems also seriously undermine the body’s ability to digest food, absorb certain vitamins, and produce hormones which regulate metabolism. Alcohol contains calories, reducing the patient’s feeling of hunger, so he/she consequently may not eat enough proper food to supply the body with essential nutrients.
In the poorer nations malnutrition is commonly caused by:
- Food shortages – in the poorer developing nations food shortages are mainly caused by a lack of technology needed for higher yields found in modern agriculture, such as nitrogen fertilizers, pesticides and irrigation. Food shortages are a significant cause of malnutrition in many parts of the world.
- Food prices and food distribution – it is ironic that approximately 80% of malnourished children live in developing nations that actually produce food surpluses (Food and Agriculture Organization). Some leading economists say that famine is closely linked to high food prices and problems with food distribution.
- Lack of breastfeeding – experts say that lack of breastfeeding, especially in the developing world, leads to malnutrition in infants and children. In some parts of the world mothers still believe that bottle feeding is better for the child. Another reason for lack of breastfeeding, mainly in the developing world, is that mothers abandon it because they do not know how to get their baby to latch on properly, or suffer pain and discomfort.
Medical conditions
Medical conditions that can contribute to malnutrition include:
- a condition that causes a lack of appetite, such as cancer, liver disease, persistent pain or nausea
- a mental health condition, such as depression or schizophrenia, which may affect your ability to look after yourself
- a health condition that requires frequent hospital admissions
- a health condition that disrupts your body’s ability to digest food or absorb nutrients, such as Crohn’s disease or ulcerative colitis
- dementia – people with dementia may be unable to communicate their needs when it comes to eating
- a health condition that makes swallowing painful or difficult (known as dysphagia)
- persistent diarrhoea
- persistent vomiting
- taking many different types of medication at the same time – there are more than 250 types of medicine known to disrupt the body’s ability to absorb and then break down nutrients
- your body has an increased demand for energy, for example if it is trying to heal itself after major surgery or a serious injury such as aburn – or if you experience involuntary movements, such as atremor
- an eating disorder, such as anorexia nervosa
Physical factors
Physical factors can contribute to malnutrition. For example:
- If your teeth are in a poor condition, or if dentures don’t fit properly, eating can be difficult or painful.
- You may lose your appetite as a result of losing your sense of smell and taste.
- You may have a physical disability or other impairment that makes it difficult for you to cook or shop for food yourself.
Social factors
Social factors that can contribute to malnutrition include:
- living alone and being socially isolated
- limited knowledge about nutrition or cooking
- reduced mobility
- alcohol or drug dependency
- low income or poverty
Management
The Government of India has launched several programs to converge the growing rate of under nutrition children.
Midday meal scheme in Indian schools
The Akshaya Patra Foundation runs the world’s largest NGO-run midday meal program serving freshly cooked meals to over 1.3 million school children in government and government-aided schools in India. This program is conducted with part subsidies from the Government and partly with donations from individuals and corporations. The meals served by Akshaya Patra complies with the nutritional norms given by the government of India and aims to eradicate malnutrition among children in India. The midday meal programme was started on 15 August 1995.
Integrated child development scheme
The Government of India has started a program called Integrated Child Development Services (ICDS) in the year 1975. ICDS has been instrumental in improving the health of mothers and children under age 6 by providing health and nutrition education, health services, supplementary food, and pre-school education.TheICDS national development program is one of the largest in the world. It reaches more than 34 million children aged 0–6 years and 7 million pregnant and lactating mothers. Other programs impacting on under-nutrition include the National Midday Meal Scheme, the National Rural Health Mission, and the Public Distribution System (PDS). The challenge for all these programs and schemes is how to increase efficiency, impact and coverage.
National Children’s Fund
The National Children’s Fund was created during the International Year of the Child in 1979 under the Charitable Endowment Fund Act, 1890. This Fund Provides support to the voluntary organisations that help the welfare of kids.
National Plan of Action for Children
India is a signatory to the 27 survival and development goals laid down by the World Summit on children 1990. In order to implement these goals, the Department of Women & Child Development has formulated a National Plan of Action on Children. Each concerned Central Ministries/Departments, State Governments/U.Ts. and Voluntary Organisations dealing with women and children have been asked to take up appropriate measures to implement the Action Plan. These goals have been integrated into National Development Plans. A Monitoring Committee under the Chairpersonship of Secretary (Women & Child Development) reviews the achievement of goals set in the National Plan of Action. All concerned Central Ministries/Departments are represented on the Committee.
15 State Govts. have prepared State Plan of Action on the lines of National Plan of Action specifying targets for 1995 as well as for 2000 and spelling out strategies for holistic child development.
United Nations Children’s Fund
India is associated with UNICEF since 1949 and is now in the fifth decade of cooperation for assisting most disadvantaged children and their mothers. Traditionally, UNICEF has been supporting India in a number of sectors like child development, women’s development, urban basic services, support for community based convergent services, health, education, nutrition, water & sanitation, childhood disability, children in especially difficult circumstances, information and communication, planning and program support.
Diagnosis
Prompt diagnosis is key to preventing complications. There are several ways of identifying adults who are malnourished, at risk of malnutrition, or obese. Below is BAPEN’s (British Association for Parenteral and Enteral Nutrition’s) MUST (Malnutrition Universal Screening Tool) – a quick to use screening tool to identify those at risk of malnutrition:
MUST (Malnutrition Universal Screening Tool)
MUST has been designed to identify adults, especially elderly people, who are:
- Malnourished
- At risk of malnutrition (under nutrition)
- Obese.
MUST also includes management guidelines which can be used to develop a care plan. It is a five-step tool for use in hospitals, community and other care settings and can be used by all care workers to identify those at risk from malnutrition.
MUST 5-step plan:
- Step 1 – Measure height and weight to get a BMI (body mass index) score.
- Step 2 – Note percentage unplanned weight loss and score.
- Step 3 – Establish acute disease (any underlying illness, such as a psychological condition) effect and score.
- Step 4 – Add scores from steps 1, 2 and 3 together to obtain overall risk of malnutrition.
- Step 5 – Use management guidelines and/or local policy to develop care plan.
MUST is only used for identifying malnutrition or risk of malnutrition in adults. It is not designed to identify deficiencies/excesses in vitamin and/or mineral intake.
- STEP 1 (BMI kg/m2 Score)
BMI >20 (>30 obese), score 0
BMI 18.5 to 20 – score 1
BMI <18.5 – score 2
If there are problems measuring BMI: If height cannot be measured – use recently documented or self-reported height (if reliable and realistic). If the subject does not know or is unable to report their height, use one of the alternative measurements to estimate height (ulna, knee height or demispan).
If height and weight cannot be obtained – use mid upper arm circumference (MUAC) measurement to estimate BMI category.
- STEP 2 (Weight Loss Score)
Unplanned weight loss in past 6 months
<5% – score 0
5% to 10% – score 1
>10% – score 2
If recent weight loss cannot be calculated, use self-reported weight loss (if reliable and realistic).
- STEP 3 (Acute Disease Effect Score) : If the patient is acutely ill and there has been or is likely to be no nutritional intake for over 5 days – score 3
- STEP 4 (Overall Risk of Malnutrition)
STEP 1 + STEP 2 + STEP 3 = STEP 4
Add Scores together to calculate overall risk of malnutrition
Low Risk – Score 0
Medium Risk – Score 1
High Risk – Score 2 or more
- STEP 5 – Management Guidelines
- Low risk, score 0
Repeat hospital screening weekly
Repeat care home screening monthly
Repeat community screening annually for special groups, e.g. those age over 75 years
Medium risk, score 1
Observe
Document dietary intake for 3 days if subject is in hospital or care home.
If improved or adequate intake – little clinical concern; if no improvement – clinical concern – follow local policy.
Repeat hospital screening weekly
Repeat care home screening at least monthly
Repeat community screening at least every 2 to 3 months
- High risk, score 2 or more
Treat (Unless detrimental or no benefit is expected from nutritional support e.g. imminent death)
Refer to dietitian, Nutritional Support Team, or implement local policy.
Improve and increase overall nutritional intake
Monitor and review care plan:
Hospital – weekly
Care home – monthly
Community – monthly.
All risk categories:
Treat underlying condition and provide help and advice on food choices, eating and drinking when necessary.
Record malnutrition risk category.
Record need for special diets and follow local policy.
Obesity:
Record presence of obesity. For those with underlying conditions, these are generally controlled before the treatment of obesity.
Subjective criteria
If height, weight or BMI cannot be obtained, the following criteria which relate to them can assist your professional judgment of the subject’s nutritional risk category. Use of these criteria is not designed to assign a score.
- BMI – clinical impression: thin, acceptable weight, overweight. Obvious wasting (very thin) and obesity (very overweight) can also be noted.
- Unplanned weight loss – clothes and/or jewelry have become loose fitting (weight loss). History of decreased food intake, reduced appetite or swallowing problems over 3-6 months and underlying disease or psycho-social/physical disabilities likely to cause weight loss.
- Acute disease effect – no nutritional intake or likelihood of no intake for more than 5 days.
Treatment options
Treatment is necessary if you or your child have any changes in the body’s ability to function. Contact your health care provider if the following symptoms develop:
- Fainting
- Lack of menstruation
- Lack of growth in children
- Rapid hair loss
The type of malnutrition treatment recommended depends mainly on its severity, and whether the patient has an underlying condition/illness which is a contributory factor. If so, that underlying illness/condition needs to be treated or addressed.
NICE (National Institute for Health and Clinical Excellence), UK, has guidelines for malnutrition treatment.
They state that the needs and preferences of the patient need to be taken into account. The patient, along with healthcare professionals, should be able to make informed decisions about care and treatment.
NICE guidelines say that individuals who are receiving nutritional support, as well as their caregivers (UK: carers):
- Should be fully informed about their treatment
- Should be given tailored information
- Should be given the opportunity to discuss diagnosis, treatment options and relevant physical, psychological and social issues.
- Should be given contact details of relevant support groups, charities and voluntary organizations.
When a diagnosis of either malnutrition or malnutrition risk has been made, the healthcare professional (either a doctor or dietician) who is responsible for the patient will devise a targeted care plan.
The care plan – aims for treatment will be set out, which should include the treatment for any underlying conditions/illnesses which are contributory factors to the malnutrition.
Typically, treatment will include a feeding program with a specially planned diet, and possibly some additional nutritional supplements.
Severely malnourished patients, or individuals who cannot get sufficient nutrition by eating or drinking may need and should receive artificial nutritional support.
The patient will be closely monitored for progress. Their treatment will be regularly reviewed to make sure their nutritional needs are being met.
Diet – a good healthcare professional will discuss eating and drinking with the patient and provide advice regarding healthy food choices. The aim is to make sure the patient is receiving a healthy, nutritious diet.
The doctor or dietitian will work with the patient to make sure enough calories are being consumed from carbohydrates, proteins, fats and diary, as well as vitamins and minerals. If the patient cannot get their nutritional requirements from the food they eat, oral supplements may be needed. An additional 250kcal to 600kcal may be advised.
Artificial nutritional support – there are two main types of artificial nutritional support, mainly for patients with severe malnutrition:
- Enteral nutrition (tube feeding) – a tube is placed in the nose, the stomach or small intestine. If it goes through the nose it is called a nasogastric tube or nasoenteral tube. If the tube goes through the skin into the stomach it is called a gastrostomy or percutaneous endoscopic gastrostomy (PEG) tube. One that goes into the small intestine is called a jejunostomy or percutaneous endoscopic jejunostomy (PEJ) tube.
- Parenteral feeding – a sterile liquid is fed directly into the bloodstream (intravenously). Some patients may not be able to take nourishment directly into their stomach or small intestine.
Monitoring progress – the patient will be regularly monitored to check that he/she is receiving the right amount of calories and nutritional needs. This may be adjusted as the patient’s requirements change. Patients receiving artificial nutritional support will be switched over to normal eating as soon as they are able to.
Preventing malnutrition
Malnutrition is caused mainly by not consuming “the right balance of nutrients from major food groups”.
These include:
- Carbohydrates
- Fruit and vegetables
- Protein
- Dairy – vegans are able to find abundant nutrients from non-animal sources
- Fats.
The average human should drink at least 1.2 liters of fluid per day.
- Ulcerative colitis – a fairly common chronic (long-term) disease that causes inflammation of the colon (the large intestine). It is a form of inflammatory bowel disease. When inflammation is only in the rectum the disease is called ulcerative proctitis. The inflammation may extend into the upper parts of the colon. Universal colitis orpancolitis is when the whole colon is involved.
Patients with ulcerative colitis commonly lose weight because their body is unable to absorb nutrients properly. Consuming plenty of fluids, and eating regularly (five or six small meals daily), as well as taking food supplements may help to prevent ulcerative colitis. - Crohn’s disease – an ongoing condition that causes inflammation of the digestive tract, or the GI (gastrointestinal) tract (the gut). Crohn’s disease may also be called ileitis or enteritis. Crohn’s disease can affect any part of the gut, from the mouth all the way down to the anus. In the majority of cases the lower part of the small intestine – the ileum – is affected. Patients with Crohn’s disease can feel pain; the condition makes the intestines empty frequently, resulting in diarrhea. Although preventing Crohn’s disease is unlikely, following treatment carefully helps prevent malnutrition considerably.
- Celiac disease – also known as gluten intolerance. If you suffer from Celiac disease you have a genetic disorder that makes you intolerant to gluten. It is caused by a reaction to gliadin (a gluten protein found in wheat). It can affect all types of people. However, it seems to be more prevalent among people of Northern European descent. Patients who follow a well-balanced, healthy, gluten-free diet are less likely to suffer from malnutrition.
- Alcohol abuse – people who are addicted to alcohol and abuse alcohol may sometimes suffer from malnutrition. The only effective way to address this is to treat the alcoholism. There are several ways of treating alcoholism. The first step for the alcoholic it to acknowledge that there is an alcohol dependency problem. The next step is to get help.
Reference sources:
1) Wikipedia
3) http://www.ifpri.org/publication/2009-global-hunger-index

