WHO Declares Mpox Outbreak A Public Health Emergency Of International Concern
This year, in 2024 Mpox (formerly known as monkeypox) is causing significant concern, particularly in Africa, where the outbreak has surged to unprecedented levels. Since January, over 2,000 cases and thirteen deaths have been reported in 15 African countries, with the Democratic Republic of the Congo (DRC) experiencing the brunt of the outbreak. A new and highly transmissible variant of the virus, clade 1b, has been identified, further escalating the crisis.
The World Health Organization (WHO) declared the outbreak a Public Health Emergency of International Concern (PHEIC) on August 14, 2024,. The WHO has since launched an international response plan, seeking $135 million to control and stop the outbreak.
More about Monkeypox or Mpox:
Mpox, formerly known as monkeypox, is a viral disease caused by the monkeypox virus (MPXV), which belongs to the same family of viruses as smallpox (Orthopoxvirus). It primarily affects animals, but it can be transmitted to humans.
‘Mpox is a zoonosis, a disease that is transmitted from animals to humans, with cases often found close to tropical rainforests where there are animals that carry the viruses’ (WHO)
Symptoms of Mpox:
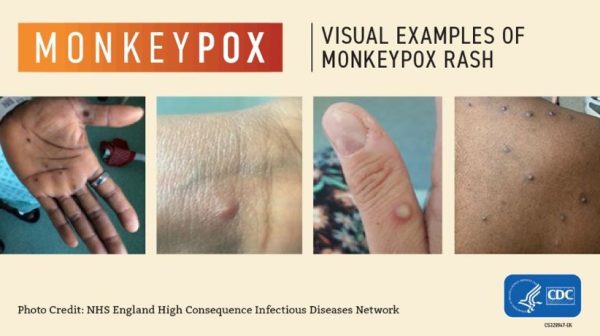
- Rash or lesions: Often the most visible symptom, starting as flat red spots that evolve into raised bumps, blisters, and finally scabs.
- Fever
- Headache
- Muscle aches
- Swollen lymph nodes
- Fatigue
The illness typically lasts for 2 to 4 weeks, with most patients recovering without severe complications.
Transmission of Mpox: Mpox spreads through close physical contact with:
- Infected persons: Direct skin-to-skin contact with the rash, scabs, or bodily fluids of someone infected.
- Contaminated objects: Touching clothing, bedding, or other materials that have been used by an infected individual.
- Respiratory droplets: Prolonged face-to-face contact can lead to transmission through respiratory droplets.
- Animals: Direct contact with infected animals (e.g., monkeys, rodents) or consuming their meat.
Though it is not as contagious as some other viral diseases, the spread within communities, especially those with close contact or shared living spaces, can lead to outbreaks.
Testing for Mpox virus:
Detection of viral DNA by polymerase chain reaction (PCR) is the preferred laboratory test for mpox. The best diagnostic specimens are taken directly from the rash – skin, fluid or crusts, or biopsy where feasible.
- PCR (Polymerase Chain Reaction): This is the gold standard for detecting the monkeypox virus. It amplifies the viral DNA from the sample, allowing for highly accurate identification.
- Viral Culture: In some cases, the virus can be grown in a laboratory to confirm infection, although this is less commonly used than PCR due to the time and complexity involved.
- Antigen Tests: These tests detect viral proteins from the monkeypox virus, though they are not as widely available or as accurate as PCR.
- Serology: This blood test detects antibodies against the monkeypox virus. However, it is more useful for understanding past exposure rather than diagnosing active infection.
Prevention and precautions:
Prevention methods include avoiding contact with infected individuals, proper hygiene, using personal protective equipment, and in some cases, smallpox vaccines which may offer some protection against mpox.
To prevent the spread of mpox, it is important to take the following precautions:
1. Avoid close contact:
- Infected Individuals: Avoid direct skin-to-skin contact with anyone who has a rash or lesions consistent with mpox.
- Contaminated Objects: Refrain from touching clothing, bedding, or personal items that have been used by an infected person.
2. Practice good hygiene
- Handwashing: Wash hands frequently with soap and water, especially after contact with potentially infected people or materials.
- Hand Sanitizers: Use alcohol-based hand sanitizers if soap and water are not available.
3. Use personal protective equipment (PPE):
- Face Masks: Wear a mask when near someone who might be infected, especially in situations where prolonged face-to-face contact is unavoidable.
- Gloves: Wear gloves if you need to handle the belongings of someone who may be infected or if you are caring for someone with mpox.
4. Isolate infected individuals:
- Quarantine: Those diagnosed with mpox should be isolated from others until all lesions have scabbed over and new skin has formed.
- Dedicated Space: In households, infected individuals should use a separate room and bathroom if possible.
5. Disinfect surfaces:
- Cleaning: Regularly disinfect surfaces, especially in areas where an infected person has spent time. Use appropriate cleaning agents that kill viruses.
6. Avoid contact with animals:
- Wildlife: Avoid contact with animals that could harbor the virus, such as rodents or non-human primates.
- Pets: Keep pets away from sick individuals as the virus can spread between animals and humans.
7. Vaccination:
- Smallpox Vaccine: The smallpox vaccine has been shown to offer some protection against mpox. In certain high-risk populations or areas experiencing outbreaks, vaccination may be recommended.
8. Travel precautions:
- Monitor Travel Advisories: Be aware of any travel advisories related to mpox outbreaks, especially when visiting areas where the virus is endemic.
- Health Monitoring: If you have traveled to an area with an outbreak, monitor your health for symptoms for up to 21 days and avoid close contact with others during this time.
9. Early detection and treatment:
- Seek Medical Attention: If you develop symptoms consistent with mpox, contact a healthcare provider promptly. Early diagnosis and supportive care can help prevent complications and limit the spread of the virus.
By following these precautions, the spread of mpox can be minimized, protecting both individuals and communities.
References:
https://news.un.org/en/story/2024/08/1153511
Image credit: NHS England High Consequence Disease Network, CDC
Author: Sumana Rao | Posted on: August 26, 2024
« Brain Eating Amoeba Reported In Kerala, India Travel Alert – Oropouche Virus Outbreak in Americas And Precautions For Public And Pregnant Women »




















Write a comment